Misdiagnosis Lawyer NYC - Delayed Diagnosis Attorney New York
 The New York medical misdiagnosis attorneys at Gair, Gair, Conason, Rubinowitz, Bloom, Hershenhorn, Steigman & Mackauf represented hundreds of clients who have been injured or have died as the result of a delayed or wrong diagnosis . Based in Manhattan, the firm handles cases throughout New York and has achieved verdicts and settlements that are among the largest in the State.
The New York medical misdiagnosis attorneys at Gair, Gair, Conason, Rubinowitz, Bloom, Hershenhorn, Steigman & Mackauf represented hundreds of clients who have been injured or have died as the result of a delayed or wrong diagnosis . Based in Manhattan, the firm handles cases throughout New York and has achieved verdicts and settlements that are among the largest in the State.
Cases we handle include among others:
- Influenza Misdiagnosis
- Failure to Treat Heart Attack (Acute Myocardial Infarction)
- Failure to Diagnose Hydrocephalus
- Failure to diagnose Compartment Syndrome
- Wrong Diagnosis of Tuberculosis
- Strokes Misdiagnosis
- Failure to diagnose Pulmonary Embolism
- Diabetes Misdiagnosis
- Bacterial Meningitis Misdiagnosis
- Delayed diagnosis of Appendicitis
- Cancer Misdiagnosis
If you have gone to a doctor, emergency room, or other medical facility with complaints of pain or other complaints indicative of a possible serious underlying disease or acute medical problem and the doctor does not do tests, such as radiology studies which are indicated based on your complaints but simply ignores your complaints and does not properly investigate your condition and you are subsequently diagnosed with a serious illness that could have been promptly treated you may have a case if the failure to diagnose your condition caused it to become worse. You may also have a failure to diagnose case if a doctor did not properly interpret a radiology study causing your condition to progress causing you injury. There are many types of failure to diagnose claims. This is meant as a brief overview.
Whether a doctor or hospital staff is at fault, a misdiagnosis of a serious illness can have extreme effects on a patient’s life. The attorneys at the Manahattan personal injury law firm of Gair, Gair, Conason, Rubinowitz, Bloom, Heshenhorn, Steigman and Mackauf are well-versed in the latest developments in medical practices and can identify any deviation in care. Our team of attorneys includes 2 board-certified physicians who can assist to review your case, and help you to understand the full medical scope of your injury. Our firm conducts exhaustive investigations and we retain extremely qualified experts to bring a comprehensive level of expertise to surpass that on the other side. For example, when a doctor fails to diagnose breast cancer, we seek out and retain a practicing Breast Cancer Specialist to determine the full circumstances of the misdiagnosis and in the case of a misread mammogram, we will find an expert radiologist to examine a your x-rays.
If necessary, we also retain expert accountants and financial analysts because many medical malpractice cases have their own set of associated losses including lost wages, the cost of care and many other monetary costs. In order to accurately assess what these costs will be for the remainder of a victim’s life, we use financial professionals to derive fair resolutions for injury victims.
Our firm's misdiagnosis lawyers have achieved many substantial settlements and verdicts for our clients. Some notable results include:
- $120,000,000 verdict awarded to a 41-year-old man whose doctors failed to diagnose and timely treat a stroke he was suffering from. As a result, this young father suffered irreversible brain damage and will spend the rest of his life in a memory care center
- $90,939,857 jury verdict for a child whose cerebral palsy was due to the failure of an obstetrician to diagnose placental abruption and who thus delayed the cesarean section that was necessary to rescue the baby who was suffering from a lack of oxygen.
- $17,250,000 verdict for a man who was rendered partially incontinent as a result of medical malpractice in failing to diagnose a spinal malformation.
- $9,200,000 settlement in a Brooklyn medical malpractice case in which doctors and hospital employees fail to timely diagnose and treat a small bowel obstruction which resulted in systemic infections, multiple surgeries, lengthy hospitalization, and the need for a kidney transplant.
- $7,000,000 award for a 35-year-old Brooklyn bookkeeper who was misdiagnosed with Bell’s Palsy in a Brooklyn emergency room while suffering an evolving stroke.
- $8,000,000 settlement for a woman in case in which doctors and hospital employees failed to timely diagnose a valvulus (twisting of the intestine) in a woman which cased multiple surgeries and hospitalizations and the need for an intestinal transplant.
- $4,750,000 settlement in an obstetrical malpractice case in which a baby’s brain damage was due both to the obstetrician’s failure to diagnose fetal distress during labor and to the pediatricians’ failure to resuscitate the newborn baby properly.
- $4,500,000 settlement in a legal malpractice case involving a woman whose lawyer failed to file the proper paperwork with the court when she had a claim against her doctor for failing to properly treat her brain tumor.
- $4,000,000 recovery for a Kings County man who was admitted to the emergency room after a bar fight and had sustained an undiagnosed subdural hematoma.
- $3,500,000 settlement for a 15-month-old diagnosed with Neurofibromatosis Type 1 (NF-1), due to medical negligence in failing to conduct necessary neuroimaging, allowing a tumor to grow undetected.
- $3,450,000 million settlement in a New York Metro wrongful death lawsuit due to medical professionals' oversight in diagnosing a pneumothorax and internal bleeding.
- $3,000,000 million settlement, the full policy limit, for the wrongful death of a 56-year-old due to an urgent care's failure to diagnose an aortic dissection.
- $3,000,000 settlement for the estate of a woman who died during childbirth as a result of the physician's failure to diagnose internal bleeding.
- $3,000,000 recovery in a New York Medical Malpractice case for an 18 year old girl who lost her leg as a result of a physician's malpractice in failing to diagnose a pseudoaneurism of the popliteal artery following an ACL repair. This was the full amount of insurance coverage.
- $2,800,000 settlement against an optician on behalf of man who suffered legal blindless as a result of a the optician’s failure to refer him to a specialist for treatment of proliferative diabetic retinopathy.
- $2,750,000 settlement in a medical malpractice wrongful death case due to the failure to diagnose toxic megacolon in a 76-year-old unmarried woman, leading to septic shock and death.
- $2,700,000 settlement in a medical malpractice case claiming a failure to administer anti-coagulation medication to a 78 year old woman following surgery resulting in a stroke.
- $2,300,000 settlement on behalf of a woman whose doctors failed to timely diagnose her breast cancer.
- $2,300,000 settlement for a Nassau County woman whose 58-year-old husband died from an untreated bacterial infection. Emergency room doctors failed to conduct a thorough history and examination, allowing the infection to advance and result in his death.
- $2,250,000 settlement in an Erie County medical malpractice case in which doctors failed to timely diagnose and treat acute gastrointestinal bleeding in a 60 year old man.
- $2,200,000 settlement for a man whose physician caused a one day delay in diagnosing a brain tumor.
- $2,175,000 on behalf of a man whose wife died because her doctors failed to diagnose her benign meningoma.
- $2,175,000 settlement millin a medical malpractice case in which doctors it was claimed that there was a failure to diagnose a meningioma
- $2,000,000 settlement in medical malpractice case involving the failure to diagnose breast cancer.
- $1,950,000 settlement for a man in a medical malpractice case stemming from a Mt. Sinai doctor's failure to diagnose bladder cancer.
- $1,900,000 settlement in a Richmond County medical malpractice case in which doctors failed to diagnose preeclampsia in a woman suffered a cerebral bleed a few days after giving birth
- $1,850,000 recovery in a New York medical malpractice case for the death of a single man for failure to diagnose malfunction of a ventricular peritoneal shunt.
- $1,750,000 settlement in a medical malpractice case in which doctors failure to diagnose colon cancer in a 67 year old man.
- $1,700,000 settlement in a medical malpractice case in which am ophthalmologist failed to timely diagnose and treat a post-cataract surgery infection resulting in loss of vision in an eye.
- $1,650,000 settlement in a failure to diagnose thoracic myelopathy lawsuit.
- $1,600,000 settlement in a medical malpractice case involving the failure to take an adequate biopsy of a patients ulcer and thereby failure to diagnose gastric cancer.
- $1,600,000 settlement in a medical malpractice case in which a gynecologist failed to perform a prophylactic oopherectomy on a woman who developed ovarian cancer and who had suffered breast cancer and had a positive family history of ovarian cancer.
- $1,600,000 recovery for a New York County 74-year-old woman whose lung cancer was undiagnosed but appeared in a routine chest x-ray. A $1,575,000 verdict on behalf of a woman whose doctors failed to make a timely diagnosis of her breast cancer.
- $1,450,000 for a woman whose doctors were negligent in failing to diagnose her breast cancer.
- $1,450,000 settlement in an Ulster County medical malpractice case in which doctors failed to timely diagnose a woman’s breast cancer
- $1,450,000 settlement in a Dutchess County medical malpractice case in which doctors failed to timely diagnose breast cancer.
- $1,000,000 settlement on behalf of a young boy whose doctors failed to diagnose osteomyelitis infection of his hip.
- $1,000,000 settlement on behalf of a man whose doctors failed to diagnose prostate cancer.
- $1,000,000 settlement (insurance policy limits) on behalf of a woman whose husband died because his doctor failed to timely diagnose lung cancer.
- $1,000,000 settlement (insurance policy limits) on behalf of a man whose doctors failed to diagnose colon cancer. A $1,350,000 verdict for a man who suffered loss of vision in one eye and decreased vision in the other eye as a result of his doctor's failure to treat proliferative diabetic retinopathy.
- $1,000,000 (insurance policy limits) settlement for a woman whose doctors failed to properly reduce her fractured ankle.
- $1,000,000 settlement in a Broome County medical malpractice case involving the failure to timely diagnose melanoma.
 Our firm recently achieved a settlement of $1,200,000 in a medical malpractice case involving the failure to diagnose perforation of a “J-Pouch,” following a surgery for a restorative proctocolectomy with an ileorectal anastomosis and creation of the J-Pouch, all described below.
Our firm recently achieved a settlement of $1,200,000 in a medical malpractice case involving the failure to diagnose perforation of a “J-Pouch,” following a surgery for a restorative proctocolectomy with an ileorectal anastomosis and creation of the J-Pouch, all described below.
In this case, we represented a young man suffering from ulcerative colitis, an inflammatory disease of the large intestine (also known as the colon or large bowel) that causes sores or ulcerations of the colon lining. The ulcers cause pus and mucus to form, which may result in pain and frequent bowel movements. Here, our client had been treated with steroids and other medications for many years but, upon reaching his late teens, medical treatment was no longer effective and he was left in constant pain and unable to control bowel movements. At the recommendation of a colorectal surgeon, our client underwent surgery consisting of a restorative proctocolectomy with an ileorectal anastomosis and creation of a J-pouch.
To generally summarize, this surgery involves removal of the large intestine and rectum (the last section of the large intestine ending at the anus), leaving the rectal stump. After cutting into the ileum (the last part of the small intestine), the ileum is folded back; the free sides are stapled together to form a pouch, which is then sutured to the rectal stump in a process called “anastomosis.” A rectal tube is placed through the anus into this pouch, allowing the pouch to empty feces, blood, or mucus without distending (expanding), similar to a urinary catheter. This rectal tube extended out of the pouch at the rectum and drained into a collection bag placed on the floor.
To ensure proper drainage, the rectal tube must be flushed on a regular basis; this involves disconnecting the end of the rectal tube from the tubing attached to the drainage bag, inserting a bulb syringe containing saline into the rectal tube, and then injecting the saline into the rectal tube. A review of the hospital chart in this case revealed the tube was flushed by a nurse daily, usually at 5:00 a.m.
Based on nursing notes in our client’s medical chart, it was clear that the J-Pouch had been perforated by the rectal tube, during a daily flush one morning – just three days after surgery. A nursing note from the afternoon (of the same day) reflected that our client had complained of severe pain that morning, after his rectal tube was flushed, and that the doctor was notified of these complaints. At his deposition, our client testified as to the extreme pain he felt at the time of the flush.
We alleged there is only one diagnosis when a patient experiences severe pain during this procedure – and that is perforation until proven otherwise. But notwithstanding his pain, the plaintiff was not seen by a physician until 12 hours after the rectal flush. He also became hypotensive (low blood pressure) and tachycardic (rapid heartbeat), with blood pressure of 80/40, (normal is 120/80) pulse 112 and pain level at incision 9 out of 10. The defendants improperly responded by calling in pain service, when they should have instead confirmed a diagnosis of perforation by ordering an emergent CT scan with radio-opaque dye through the rectal tube; this would have (if read properly) diagnosed perforation before contamination set in. Unfortunately, the pain medications masked his symptoms and resulted in a failure to treat his underlying condition thus allowing the peritonitis to become worse. Clearly, part of the failures included the decision not to listen to the patient’s complaints-a decision the likes of which have, unfortunately, resulted in many unnecessary injuries, unfortunate consequences and medical malpractice cases. We have seen all too many cases in which had the doctors taken the patient’s complaints seriously the underlying condition could have been properly treated avoiding the resulting injury.
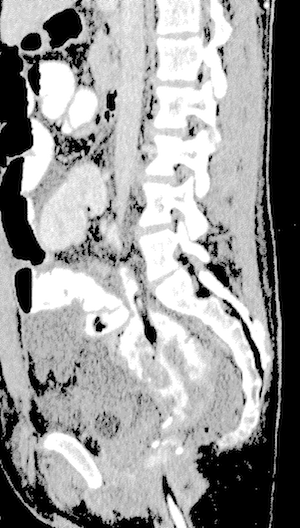
Next, when seen by the surgeon in the morning four days post-operation, our client’s white blood count was elevated to 14.9 (sign of possible infection) and he had a fever. A CT scan was performed in the early afternoon and, although it did not rule out a leak, this CT scan was misread by the attending radiologist. In particular, we consulted an expert radiologist who reviewed the CT images and opined that such images clearly show the rectal tube perforating the J-Pouch, as well as a false tract due to the perforated pouch and extravasated contrast. At the deposition of the defendant radiologist she denied that the CT images demonstrated a perforation by the rectal tube, but conceded there was a possible leak from the J-Pouch.
However, despite the obvious perforation or leak, nothing was done to address this emergent situation. The report of the CT scan failed to identify the perforated J- Pouch, and also failed to correctly identify and conclude there was a tract secondary to the perforation that was a manifestation of an ongoing leak from the J-Pouch. In addition, while considerable abdominal and pelvic fluid, free air, and small bowel abnormalities were reported, their ultimate significance, the presence of peritonitis, and its secondary manifestations on the small bowel (small intestine) were also not recognized and/or minimized, because the J-Pouch perforation was not identified.
Despite the misreading of the CT scan it did not rule out a leak. In fact, on Post-Op day four in the afternoon the surgeon noted that he had reviewed the CT with the radiology attending and noted ascites (accumulation of fluid) and inflammatory changes behind pouch. His impression was that it was a possible small leak that may have already healed. His proper response should have been to take the plaintiff urgently to the operating room for an exploratory laparotomy (surgical exploration of abdomen) which would have identified the hole which could have been repaired before the plaintiff developed severe fecal peritonitis (severe inflammation of the tissues lining the abdominal wall).
On Post-OP day 8, our client’s abdomen was distended and he had severe pain. An abdominal x-ray showed a high-grade small bowel obstruction with a massively distended stomach. A nasogastric tube was inserted to deliver food and medicine to his stomach through his nose. Another CT scan was also done and confirmed a leak.
Our client was urgently taken to the operating room by the colorectal surgeon. Although the pre-operative diagnosis was anastomotic leak (leak from suture of J-Pouch to rectal stump), the post-operative diagnosis was perforation of pelvic J-pouch. A laparotomy with washout, repair of the perforation and a diverting loop ileostomy was performed; a portion of the ileum is diverted to an opening in the abdominal wall and attached to the skin and empties feces into what is called an Ostomy bag. In surgery, a great deal of dilated small bowel as well as fibrous exudate on numerous surfaces of the small bowel was demonstrated. The post-operative findings were diffuse fecal peritonitis, intact pouch/rectal anastomosis and small perforation in the short limb of the J-pouch anteriorly away from any suture line. At his deposition, the surgeon even admitted this was a hole, not an anastomotic leak, and that it was possible the rectal tube had caused the perforation. In other words, the leak was not from the sutures connecting the J-Pouch to the rectal stump (anastomosis), but from a hole caused by the perforation of the J-Pouch by the rectal tube.
Our ClaimsIn this case, we argued that a rectal tube flush must be done judiciously in the postoperative period but, in this case, the nurse was negligent in using too much force during the flushing procedure. Had care been used in flushing the rectal tube, using the proper technique, the perforation would have been avoided. Furthermore, there was no contemporary report in the chart written by the nurse documenting the events at the time of the rectal tube irrigation, which was associated with a sudden onset of acute abdominal pain. The acute nature of the surgical emergency was not recognized and, instead, the pain service was called. The pain service also failed to recognize the acute nature of the surgical emergency and simply ramped up pain management, without questioning as to why the patient had a sudden onset of pain.
Furthermore, not only were the defendants negligent in perforating the J-Pouch, but they compounded our client’s injuries by delaying surgery until it was too late to simply repair the hole. More specifically, it was improper to manage our client expectantly, instead of emergently, and he ultimately developed severe peritonitis, requiring the above emergent surgery. Had this surgery been performed on either Post-Op day three or four following the CT scan, the perforation could have simply been closed and the catastrophic events would have been avoided. In total, our client was hospitalized for 18 days; absent the perforation, he would have been discharged within four days.
As a result of the perforation and severe fecal peritonitis, our client was also discharged with an open wound which took over 70 days to heal. While at home waiting for the wound to heal, he required debridement of the necrotic tissue and cleaning and dressing of the wound five times a week. He remained at home, except for visits to the surgeon until five months after discharge – at which time he was readmitted to the hospital for surgery consisting of dilation of pouch-anal anastomotic stricture and resection and closure of the loop ileostomy.
The defendants argued there was insufficient proof of a perforation and, rather, that the leak was more likely to be from the suture line (a known complication of the procedure). They further claimed that the delay in performing the surgery did not make a difference, as the plaintiff would have required an ileostomy in any event. The defendants also maintained that the plaintiff made an excellent recovery and the initial surgery allowed him to live a normal life. Their position was that the case had little if any value because of issues regarding liability and damages.
Overall, this was a complex case as it involved both surgical and radiological malpractice. Before commencing the case we consulted with a radiology and colorectal surgeon expert. To further prepare the case, we reviewed all available pertinent medical literature and medical records, and took extensive depositions of both the defendant colorectal surgeon and attending radiologist who failed to properly interpret the CT scan. At the surgeon’s deposition, he was forced to concede that it was not an anastomotic leak, but a perforation on the top of the J-Pouch, not close to any suture line. However, he also opined that there was no proof the hole was caused by the rectal tube and could have been caused by an expansion of the pouch which was not avoidable.
The OutcomeOn the eve of trial, the defendants requested that we go to private mediation. While we were reluctant to do so given that we did not feel that they were serious about settling the case we agreed to do so. At the mediation our feelings were borne out as the defendants took a very adamant position as to there being no liability and very little damages. However, as a result of admissions made by the defendant surgeon at his deposition, they made an offer in the low six figures.
We then showed them illustrations of the CT Scans which we had created on a computer with the assistance of our expert radiologist identifying where the Rectal Tube perforated the J-Pouch. We then told the mediator if they were not prepared to pay over one million dollars, we did not see any point in continuing the mediation.
The mediator asked us not to leave and extensive negotiations ensued. After many hours the defendants continued to state they would not pay close to one million dollars. We then advised the mediator that we would accept $1,200,000 to settle the case and to tell the defendants we were done negotiating and would leave if they did not pay that amount.
Thereafter the case was settled for $1,200,000, as a result of our meticulous preparation of the case, which included working closely with our expert radiologist to create the dramatic images of the CT Scan depicting where the rectal tube perforated the J-Pouch and our expertise in the area of medical malpractice. Given the difficult liability and limited damages this was an exceptional result. It demonstrates the need for meticulous preparation of these types of complex cases which our firm is known for. We thoroughly prepare every case we accept in the same manner. Every case is prepared as if it was going to have to go to trial. We firmly believe in the adage that cases which are prepared to be tried are usually settled while cases which are merely prepared to be settled are tried. We thus spare no expense in preparing all our cases.
Publications by Our New York Misdiagnosis Lawyers- "Failure to Diagnose Breast Cancer: The Perspective of a Patient's Attorney in Handling the Failure to Diagnose a Breast Cancer Medical Malpractice Case," 2007. Editor: Anatomy for Lawyers, New York State Bar Association, 1980 & 1981, Stephen H. Mackauf.
- "Failure to Diagnose Cancer," Law Journal Seminars-Press, 1991 & 1992, Stephen H. Mackauf.
- "Failure to Diagnose Breast Cancer," Law Journal Seminars-Press, 1993, 1995, 1998 & 1999
- "Failure to Diagnose Breast Cancer: The Trial," Law Journal Seminars, 1998 & 2000, Stephen H. Mackauf.
- "Orthopedic Malpractice: Failure to Diagnose Injury to Popliteal Artery," Medical Malpractice Law & Strategy, Vol. XVIII, No. 9, 2001, Anthony Gair.
- "Chemotherapy: Failure to Properly Treat Extravasation of Doxorubicin," in Medical Malpractice Law and Strategy, Vol. XVIII, No.10 Aug., 2000, Anthony Gair.
- "Is It Necessarily Malpractice: Failure to Revise Shunt in Hydrocephalus Patient," Medical Malpractice Law and Strategy, Vol. XVI, No. 5, March, 1999, Anthony Gair.
- "Prosecuting a Case of Failure to Diagnose Compartment Syndrome," in Medical Malpractice Law and Strategy, Vol. XV, No. 12, Oct., 1998, Anthony Gair.
- "Medical Malpractice: Failures in Cancer Diagnosis & Treatment," Law Journal Seminars-Press 1987 and 1988, Robert L. Conason (co-Author)
- "Failure to Diagnose Cancer", Law Journal Seminars-Press, 1991 and 1992, Robert L. Conason (co-Author) v"Failure to Diagnose Breast Cancer," Law Journal Seminars-Press 1993 to 1999, Robert L. Conason (co-Author)
Is Misdiagnosis Common?
Yes, misdiagnosis is unfortunately common in the United States, as highlighted by a recent study indicating that nearly 800,000 cases of permanent disability or death occur each year due to diagnostic errors. This alarming statistic reveals the devastating impact of misdiagnosed diseases and medical conditions, leading to approximately 371,000 deaths and 424,000 cases of permanent disabilities annually. The study emphasizes the prevalence of misdiagnoses for conditions like stroke, sepsis, pneumonia, venous thromboembolism, and lung cancer, which together contribute to nearly 40% of severe outcomes related to diagnostic errors. Addressing this issue requires concerted efforts to improve diagnostic accuracy, invest in research, and enhance patient engagement in their healthcare to reduce the occurrence of misdiagnoses and prioritize patient safety.
The NYC Misdiagnosis Attorneys at Gair, Gair, Conason, Rubinowitz, Bloom, Hershenhorn, Steigman & Mackauf advocate for our clients' full financial recovery through detailed, meticulous preparation for trial. If you or a loved one was injured or died as the result of a delayed or wrong diagnosis, please contact our Manhattan firm by email to discuss your case or call us at (212) 943-1090.
Disclaimer: Please be advised that the results achieved in any given case depend upon the exact facts and circumstances of that case. Gair, Gair, Conason, Rubinowitz, Bloom, Hershenhorn, Steigman & Mackauf cannot guarantee a specific result in any legal matter. Any testimonial or case result listed on this site is based on an actual legal case and represents the results achieved in that particular case, and does not constitute a guarantee, warranty or prediction of the outcome of any other legal matter.
 Gair, Gair, Conason, Rubinowitz, Bloom, Hershenhorn, Steigman & Mackauf Home
Gair, Gair, Conason, Rubinowitz, Bloom, Hershenhorn, Steigman & Mackauf Home